Medical insurance plays a crucial role in the healthcare system, allowing patients to access necessary services while minimizing financial burdens. This article provides a comprehensive overview of the revenue cycle in healthcare, including key components like patient registration, medical coding, claims processing, and more.
The Revenue Cycle in Healthcare
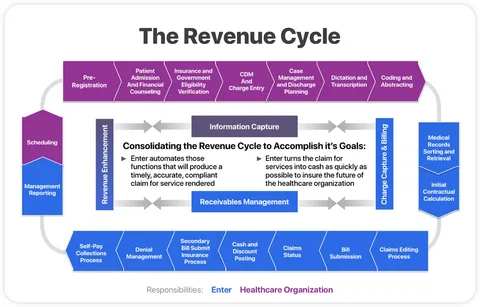
The revenue cycle encompasses all the administrative and clinical functions that contribute to the management of claims, payment, and revenue generation. It begins when a patient schedules an appointment and continues until all payments are collected. Here’s a breakdown of the key stages:
| Stage | Description |
|---|---|
| Patient Registration | Collecting patient information and insurance details |
| Insurance Verification | Confirming coverage and benefits |
| Medical Coding and Billing | Translating healthcare services into codes for billing |
| Claims Submission and Processing | Submitting claims to insurance companies |
| Payment Posting and Reconciliation | Recording payments and reconciling accounts |
| Managing Accounts Receivable | Tracking outstanding payments and collections |
| Compliance and Regulatory Considerations | Ensuring adherence to laws and regulations |
| Technological Advancements | Utilizing technology to streamline processes |
Patient Registration and Insurance Verification
The process begins with patient registration, where healthcare providers collect essential information, including:
- Patient name
- Date of birth
- Insurance details
Once registered, insurance verification follows to confirm the patient’s coverage. This step is crucial, as it can prevent future billing issues. According to the American Academy of Professional Coders, “Verification ensures that the services provided are eligible for coverage under the patient’s plan” (AAPC).
Medical Coding and Billing
Once services are provided, medical coding is performed. This involves translating diagnoses and procedures into standardized codes, such as ICD-10 and CPT codes. Effective coding is vital for accurate billing and reimbursement.
Key Points of Medical Coding:
- Accuracy: Ensures correct reimbursement.
- Compliance: Adheres to regulations and guidelines.
- Documentation: Requires thorough and precise patient records.
Claims Submission and Processing
After coding, claims are submitted to insurers for payment. This process can be complex and requires attention to detail. Common reasons for claim denials include:
- Incorrect patient information
- Coding errors
- Lack of medical necessity
To mitigate these issues, healthcare providers should implement a robust claims management system.
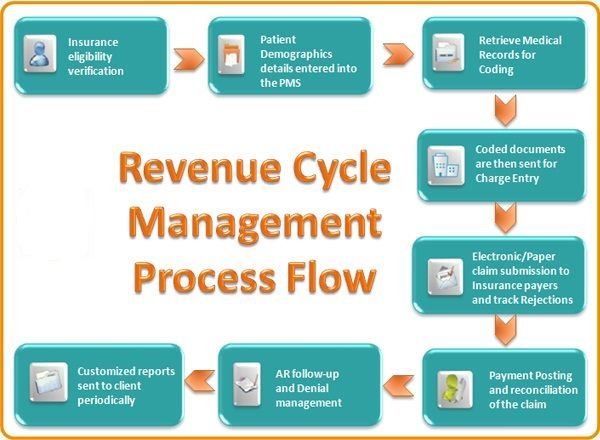
Payment Posting and Reconciliation
Once claims are processed, payments are posted to patient accounts. This step involves reconciling payments with submitted claims. Effective reconciliation helps healthcare organizations track outstanding balances and ensures accurate financial reporting.
Managing Accounts Receivable
Managing accounts receivable (AR) is crucial for maintaining cash flow. Key strategies include:
- Regular follow-up on unpaid claims
- Offering payment plans to patients
- Utilizing AR management software
A healthy AR process ensures that healthcare providers receive timely payments for services rendered.
Compliance and Regulatory Considerations
Healthcare organizations must adhere to various regulations, including HIPAA and the Affordable Care Act. Compliance is essential to avoid penalties and ensure patient data protection. Regular training and audits can help maintain compliance.
Technological Advancements in Revenue Cycle Management
Technology plays an increasingly important role in revenue cycle management (RCM). Innovations such as electronic health records (EHRs), automated billing systems, and AI-driven analytics improve efficiency and accuracy. As noted by Healthcare Financial Management Association, “Technology not only streamlines operations but also enhances patient satisfaction by reducing errors and wait times” (HFMA).
Conclusion
Understanding the revenue cycle in healthcare is essential for both providers and patients. By grasping the intricacies of patient registration, medical coding, claims processing, and more, stakeholders can ensure a smoother experience and better financial outcomes. Embracing technology will further enhance these processes, leading to improved healthcare delivery and patient satisfaction.
For more information, consider visiting the following resources:
By staying informed about the basics of medical insurance and the revenue cycle, stakeholders can navigate the complexities of healthcare with greater confidence.